Kims Hospitals, Beside Vijaya Sales, Madinaguda
+91-7799111005
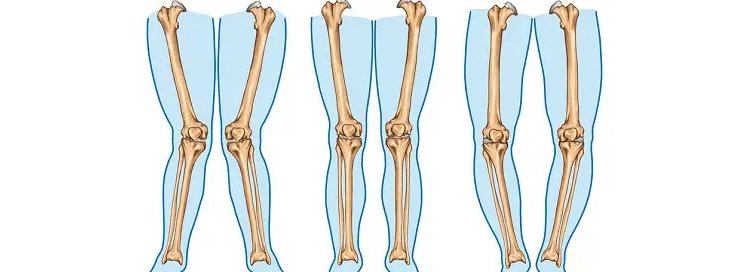
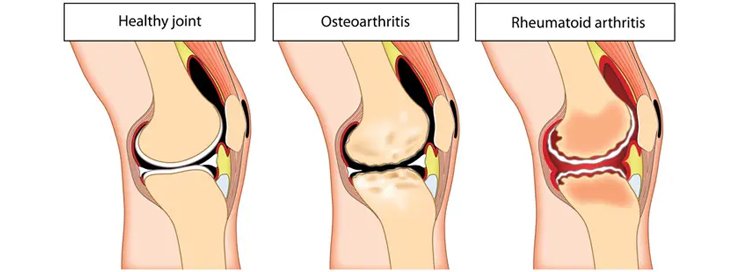
Knee deformities refer to abnormal alignment of the knee joint, leading to pain, discomfort, and mobility issues. These conditions can be congenital or develop over time due to injury, arthritis, or other orthopedic conditions. Proper diagnosis and treatment are crucial to prevent further complications and improve the quality of life.
Genu Valgum, commonly known as knock knees, is a condition where the knees angle inward and touch each other when standing straight. It is often seen in children but can persist into adulthood due to factors such as bone disorders or arthritis.
Genu Varum, or bow legs, is characterized by outward bending of the legs, causing a noticeable gap between the knees. This condition can result from nutritional deficiencies, genetic factors, or conditions like Blount’s disease.
Genu Varum, or bow legs, is characterized by outward bending of the legs, causing a noticeable gap between the knees. This condition can result from nutritional deficiencies, genetic factors, or conditions like Blount’s disease.
Genu Recurvatum occurs when the knee bends backward excessively. This condition can lead to instability, knee pain, and an increased risk of injury. It is often seen in individuals with ligament laxity or post-traumatic injuries.
Knee deformities often present with symptoms such as pain, stiffness, difficulty walking, and joint instability. Diagnosis involves a physical examination, X-rays, and MRI scans to assess the severity and underlying cause of the condition.
Consulting an experienced orthopedic doctor is essential for accurate diagnosis and treatment. Specialists in knee replacement surgery and arthroscopic surgery can offer advanced solutions tailored to individual needs.
Madinaguda
Kims Hospitals,
Mon - Sat: 9 am - 9 pm,
Sunday: 10am - 2pm.
© All rights reserved by ARUN ORTHO CARE - Designed By Venlas Group.